Case Western Reserve University lab reports 84% accuracy in predicting from initial chest scan which patients will need breathing help; planning website for UH, Cleveland VA physicians to upload scans
Researchers at Case Western Reserve University have developed an online tool to help medical staff quickly determine which COVID-19 patients will need help breathing with a ventilator.
The tool, developed through analysis of CT scans from nearly 900 COVID-19 patients diagnosed in 2020, was able to predict ventilator need with 84% accuracy.
“That could be important for physicians as they plan how to care for a patient—and, of course, for the patient and their family to know,” said Anant Madabhushi, the Donnell Institute Professor of Biomedical Engineering at Case Western Reserve and head of the Center for Computational Imaging and Personalized Diagnostics (CCIPD). “It could also be important for hospitals as they determine how many ventilators they’ll need.” 
Next, Madabhushi said he hopes to use those results to try out the computational tool in real-time at University Hospitals and Louis Stokes Cleveland VA Medical Center with COVID-19 patients.
If successful, he said medical staff at the two hospitals could upload a digitized image of the chest scan to a cloud-based application, where the AI at Case Western Reserve would analyze it and predict whether that patient would likely need a ventilator.
The dire need for ventilators
Among the more common symptoms of severe COVID-19 cases is the need for patients to be placed on ventilators to ensure they will be able to continue to take in enough oxygen as they breathe.
Yet, almost from the start of the pandemic, the number of ventilators needed to support such patients far outpaced available supplies—to the point that hospitals began “splitting” ventilators—a practice in which a ventilator assists more than one patient.
While 2021’s climbing vaccination rates dramatically reduced COVID-19 hospitalization rates—and, in turn, the need for ventilators—the recent emergence of the Delta variant has again led to shortages in some areas of the United States and in other countries.
“These can be gut-wrenching decisions for hospitals—deciding who is going to get the most help against an aggressive disease,” Madabhushi said.
To date, physicians have lacked a consistent and reliable way to identify which newly admitted COVID-19 patients are likely to need ventilators—information that could prove invaluable to hospitals managing limited supplies.
Researchers in Madabhushi’s lab began their efforts to provide such a tool by evaluating the initial scans taken in 2020 from nearly 900 patients from the U.S. and from Wuhan, China—among the first known cases of the disease caused by the novel coronavirus.
Madabhushi said those CT scans revealed—with the help of deep-learning computers, or Artificial Intelligence (AI)—distinctive features for patients who later ended up in the intensive care unit (ICU) and needed help breathing.
The research behind the tool appeared this month in the IEEE Journal of Biomedical and Health Informatics.
Amogh Hiremath, a graduate student in Madabhushi’s lab and lead author on the paper, said patterns on the CT scans couldn’t be seen by the naked eye but were revealed only by the computers.
“This tool would allow for medical workers to administer medications or supportive interventions sooner to slow down disease progression,” Hiremath said. “And it would allow for early identification of those at increased risk of developing severe acute respiratory distress syndrome—or death. These are the patients who are ideal ventilator candidates.” 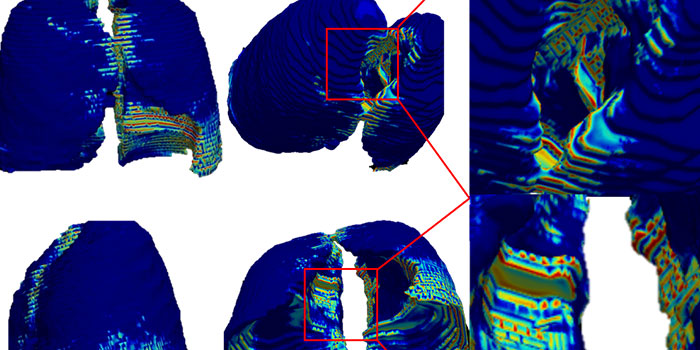
Further research into ‘immune architecture’
Madabhushi’s lab also recently published research comparing autopsy tissues scans taken from patients who died from the H1N1 virus (Swine Flu) and from COVID-19. While the results are preliminary, they do appear to reveal information about what Madabhushi called the “immune architecture” of the human body in response to the viruses.
“This is important because the computer has given us information that enriches our understanding of the mechanisms in the body against viruses,” he said. “That can play a role in how we develop vaccines, for example.”
Germán Corredor Prada, a research associate in Madabhushi’s lab who was the primary author on the paper, said computer vision and AI techniques allowed the scientists to study how certain immune cells organize in the lung tissue of some patients.
“This allowed us to find information that may not be obvious by simple visual inspection of the samples,” Corredor said. “These COVID-19-related patterns seem to be different from those of other diseases such as H1N1, a comparable viral disease.”
Eventually, when combined with other clinical work and further tests in larger sets of patients, this discovery could serve to improve the world’s understanding of these diseases and maybe others, he said.
Madabhushi established the CCIPD at Case Western Reserve in 2012. The lab now includes more than 60 researchers. Some were involved in this most recent COVID-19 work, including graduate students Hiremath, Pranjal Vaidya; research associates Corredor and Paula Toro; and research faculty Cheng Lu and Mehdi Alilou.
 How to resolve AdBlock issue?
How to resolve AdBlock issue?